Diabetes is the number one leading cause of blindness in Canada. Diabetic patients are more likely to develop cataracts, their risk is twice as high for getting Glaucoma and it could also cause Diabetic Retinopathy or Diabetic Macular Edema (DME).
What is Diabetic Retinopathy?
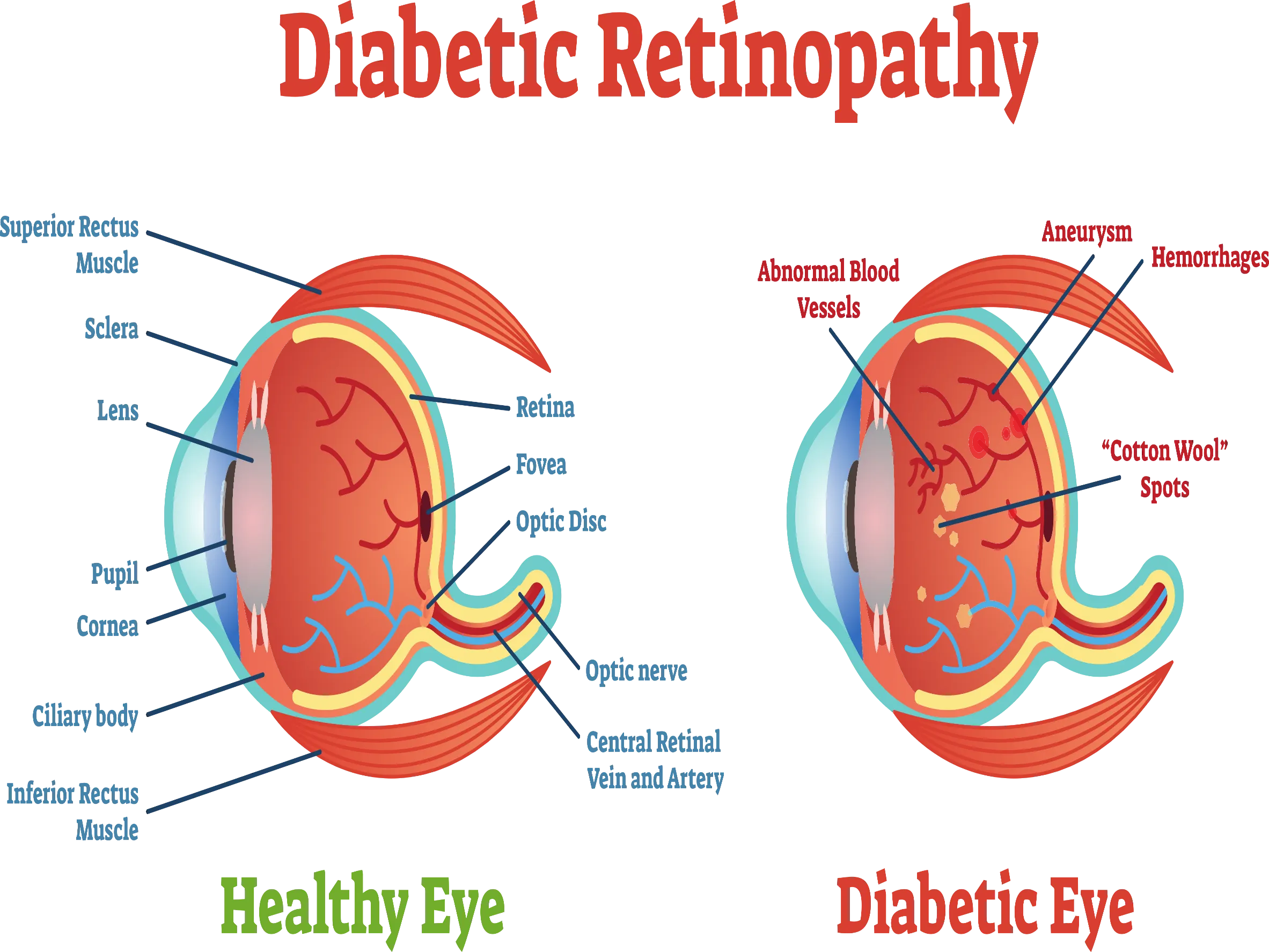
Diabetic retinopathy is a deterioration of the blood vessels in the retina that usually affects both eyes. Almost all people with uncontrolled diabetes show signs of retinal damage after they've lived about 15 to 20 years with the condition.
Diabetic Retinopathy is a complication of systemic diabetes. The damaged vessels around the retina can leak blood, protein, and fats, which can interfere with vision. The damaged blood vessels are also not as effective in carrying oxygen to the retina, which can cause further damage.
Diabetic retinopathy may progress through four stages:
- Mild nonproliferative retinopathy
- Moderate nonproliferative retinopathy
- Severe nonproliferative retinopathy.
- Proliferative diabetic retinopathy (PDR)
What is Diabetic Macular Edema (DME)?
DME is the build-up of fluid (edema) in a region of the retina called the macula. The macula is important for the sharp, straight-ahead vision that you use for reading, recognizing faces, and driving. DME is the most common cause of vision loss among people with diabetic retinopathy and around half the people with diabetic retinopathy will develop DME. Although it is more likely to occur as diabetic retinopathy worsens, DME can happen at any stage of the disease.
Prevention & Treatments
There are things you can do prevent and help manage this condition.
Prevention - Controlling blood sugar levels in diabetes is critical in delaying the onset of diabetic retinopathy. Proper management of diabetes involves taking the prescribed treatments, such as insulin or other diabetes medications, as well as following a healthy diet and exercise program.
Laser treatment (photocoagulation) – Can usually BE very effective at preventing vision loss if it is done before the retina has been severely damaged.
Surgery - If the vitreous has deteriorated, surgical removal of the vitreous gel (vitrectomy) may also help improve vision if the retina has not been severely damaged.
Anti-VEGF Injection Therapy - This therapy can reverse abnormal blood vessel growth and decrease fluid in the retina.
Treatment for diabetic retinopathy is often very effective in preventing, delaying, or reducing vision loss. But it is not a cure for the disease. People who have been treated for diabetic retinopathy need to be monitored frequently by an eye doctor to check for new changes in their eyes. Many people with diabetic retinopathy need to be treated more than once as the condition gets worse.
